There is a growing amount of evidences in favor of causative links between a chronic state of overactivity of the immune system and the development of morbidities such as atherosclerosis, metabolic syndrome and type 2 diabetes, liver steatosis, neurocognitive disorders, osteoporosis, frailty, and even some types of cancer.
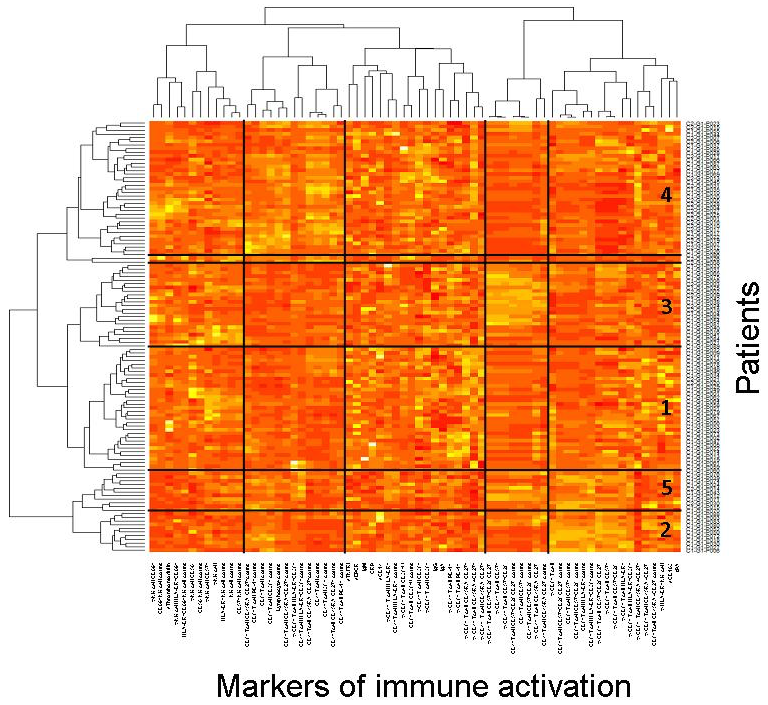
HIV infection is a relevant model to explore these causative links. Our team is working on the chronic immune activation observed in efficiently treated HIV-1 patients (virologic responders), and on its consequences. Our working hypothesis in that each virologic responder may be characterized by one out of a few profiles of immune activation. Each of these immune activation profiles could be driven by specific causes, including persistent HIV production, microbial translocation, coinfections, CD4 T cell lymphopenia, immune senescence, and/or Th17/Treg dysregulation. Moreover, each immune activation profile might fuel specific comorbidities.
Apart from driving chronic comorbidities, the persistence of immune activation in virologic responders may impede CD4 T cell recovery. We are currently exploring one mechanism linking monocyte activation to impaired CD4 T cell restoration.
Besides immune activation, another major concern for virologic responders today is the persistence of HIV genome in the so-called « reservoir cells ». Various latency-reversing agents (LRA) have been proposed to force these reservoir cells to produce virions, with the aim of inducing their destruction. After a systematic screening of G-protein coupled receptors (GPCR) coexpressed in CD4+ T cells with the HIV coreceptor CCR5, we have identified GPCR whose activation may result in reversing HIV latency.
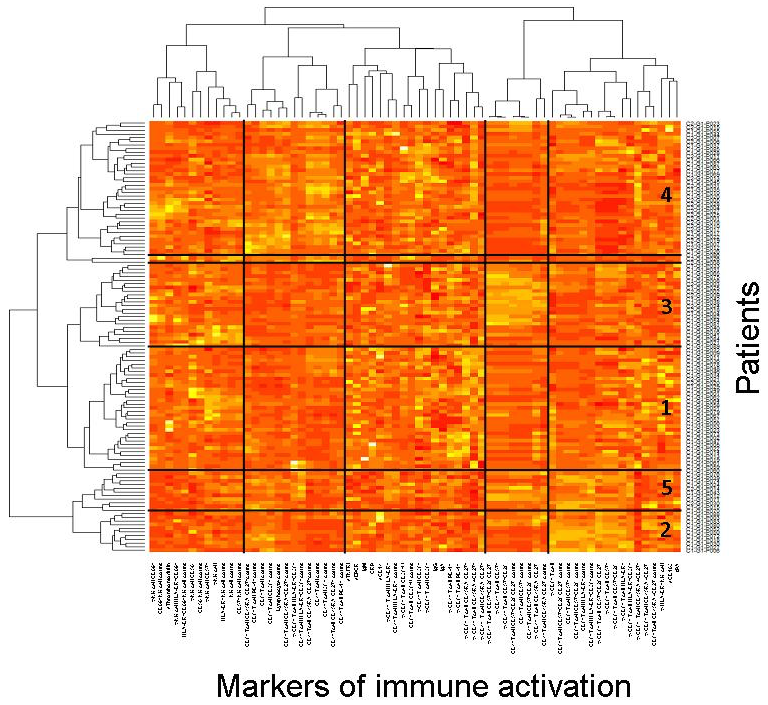
Figure 1. Virologic responders present with different immune activation profiles. Heatmap showing the hierarchical clustering of the activation markers (vertical) as well as of the virologic responders according to their profile of activation (horizontal). Each Profile number is indicated
Collaborations
- Division of Hematology, McGill University Health Center, Montréal, Québec, Canada
- Département des Maladies infectieuses et immunitaires, CHU Laval, Québec, Canada
- INSERM U1065, Nice, France
- Sorbonne Universités, UPMC Université Paris 06, INSERM, Institut Pierre Louis d’Epidémiologie et de Santé Publique (IPLESP UMRS 1136), Paris, France
- Hôpital Saint-Antoine, Département de Santé Publique, AP-HP, Paris France
- Université Paris Descartes, Sorbonne Paris Cité; AP-HP, CIC Cochin Pasteur, Hôpital Cochin, Paris, France
- INSERM, CIC 1417, Paris, F-CRIN, I–REIVAC, France